Improved Patient Outcomes
The focus on improving patient outcomes is a significant driver in the AI For Healthcare Payer Market. AI technologies facilitate personalized care by analyzing patient data to tailor treatment plans. This personalized approach not only enhances patient satisfaction but also leads to better health outcomes. Studies indicate that healthcare payers utilizing AI-driven solutions report higher rates of patient engagement and adherence to treatment protocols. As the industry shifts towards value-based care, the emphasis on outcomes will likely propel the adoption of AI technologies, making them integral to the future of healthcare delivery.
Cost Reduction Initiatives
Cost reduction remains a primary driver in the AI For Healthcare Payer Market. Healthcare payers are under constant pressure to lower operational costs while maintaining high-quality services. AI technologies offer innovative solutions that can lead to substantial cost savings. For example, predictive analytics can help in identifying high-risk patients, allowing for targeted interventions that reduce unnecessary expenditures. Reports suggest that implementing AI can lead to a reduction in costs by approximately 20 to 30% over time. As payers seek to balance cost efficiency with quality care, the integration of AI solutions is likely to become a standard practice.
Improved Operational Efficiency
The AI For Healthcare Payer Market is witnessing a surge in demand for solutions that enhance operational efficiency. By automating routine tasks such as claims processing and data entry, AI technologies can significantly reduce administrative burdens. According to recent estimates, AI-driven automation can decrease processing times by up to 30%, allowing healthcare payers to allocate resources more effectively. This efficiency not only streamlines operations but also improves the overall patient experience, as quicker claims processing leads to faster reimbursements. As healthcare payers increasingly adopt AI solutions, the industry is likely to see a transformation in how services are delivered, ultimately leading to cost savings and improved service quality.
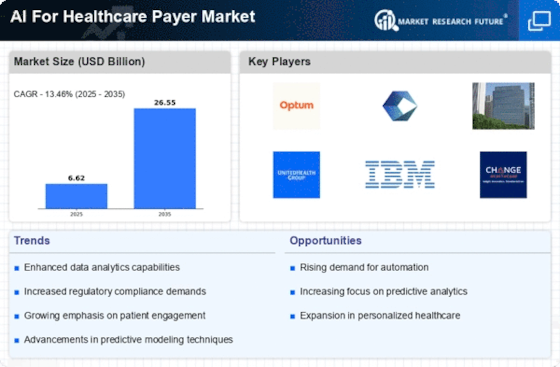
Enhanced Data Analytics Capabilities
In the AI For Healthcare Payer Market, the ability to analyze vast amounts of data is becoming increasingly critical. AI technologies enable healthcare payers to harness data analytics for better decision-making and predictive modeling. For instance, advanced algorithms can identify trends in patient behavior and treatment outcomes, which can inform policy adjustments and risk management strategies. The market for healthcare analytics is projected to grow significantly, with estimates suggesting a compound annual growth rate of over 25% in the coming years. This growth indicates a strong inclination towards data-driven strategies, which are essential for optimizing healthcare delivery and improving patient outcomes.
Regulatory Compliance and Risk Management
The AI For Healthcare Payer Market is also influenced by the need for stringent regulatory compliance and effective risk management. As regulations evolve, healthcare payers are increasingly turning to AI solutions to ensure adherence to complex compliance requirements. AI can assist in monitoring transactions and identifying potential compliance issues before they escalate. This proactive approach not only mitigates risks but also enhances the payer's reputation in the market. With the healthcare landscape becoming more regulated, the demand for AI-driven compliance solutions is expected to rise, indicating a pivotal shift in how payers manage regulatory challenges.