Increased Focus on Cost Containment
Cost containment remains a pressing concern for healthcare payers, significantly influencing the Healthcare Payer Analytics Market. With rising healthcare costs, payers are compelled to adopt analytics solutions that can identify inefficiencies and optimize resource allocation. The market is projected to grow as payers seek to implement strategies that reduce unnecessary expenditures while maintaining quality care. Analytics tools that provide insights into claims processing, fraud detection, and patient management are becoming indispensable. This focus on cost containment is expected to drive the adoption of advanced analytics solutions, thereby enhancing the overall efficiency of the Healthcare Payer Analytics Market.
Growing Importance of Patient Engagement
Patient engagement is emerging as a pivotal factor in the Healthcare Payer Analytics Market. Payers are recognizing that engaging patients in their healthcare journey can lead to improved outcomes and reduced costs. Analytics solutions that provide insights into patient behavior and preferences are becoming essential for developing effective engagement strategies. The market is anticipated to grow as payers seek to implement personalized care plans and communication strategies based on data-driven insights. By leveraging analytics to enhance patient engagement, payers can potentially improve satisfaction and adherence, which are critical for the sustainability of the Healthcare Payer Analytics Market.
Advancements in Technology and Infrastructure
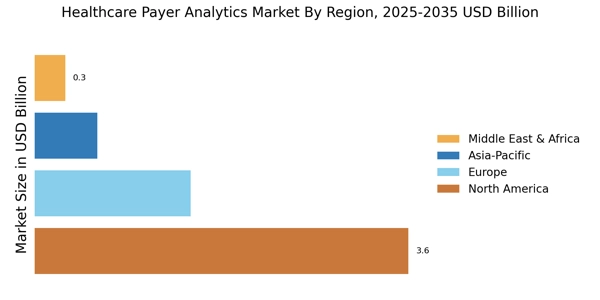
Technological advancements play a crucial role in shaping the Healthcare Payer Analytics Market. The integration of cloud computing, big data, and machine learning technologies has transformed how payers analyze and utilize data. These innovations enable real-time data processing and predictive analytics, which are essential for effective decision making. The market is expected to witness a compound annual growth rate of around 25% over the next few years, driven by these technological enhancements. As payers invest in modern infrastructure, the ability to harness vast amounts of data will likely lead to improved operational efficiencies and better patient care outcomes.
Rising Demand for Data-Driven Decision Making
The increasing emphasis on data-driven decision making within the Healthcare Payer Analytics Market is a notable driver. Payers are increasingly recognizing the value of analytics in enhancing operational efficiency and improving patient outcomes. According to recent estimates, the market for healthcare analytics is projected to reach approximately 50 billion dollars by 2026. This growth is largely attributed to the need for payers to leverage data for strategic planning, risk management, and cost reduction. As healthcare systems evolve, the demand for sophisticated analytics tools that can provide actionable insights is likely to intensify, thereby propelling the Healthcare Payer Analytics Market forward.
Regulatory Changes and Compliance Requirements
The evolving regulatory landscape is a critical driver for the Healthcare Payer Analytics Market. Payers are increasingly required to comply with stringent regulations aimed at improving transparency and accountability in healthcare. This necessitates the adoption of robust analytics solutions that can ensure compliance while also providing insights into operational performance. The market is likely to expand as payers invest in technologies that facilitate adherence to regulations such as HIPAA and the Affordable Care Act. As compliance becomes more complex, the demand for analytics tools that can streamline reporting and enhance data security will likely increase, further propelling the Healthcare Payer Analytics Market.