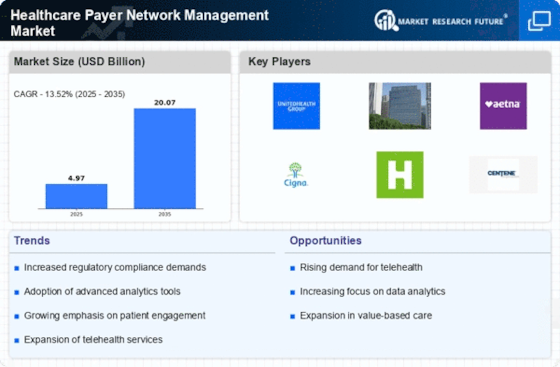
Rising Demand for Cost Efficiency
The Healthcare Payer Network Management Market is experiencing a notable shift towards cost efficiency as healthcare organizations seek to optimize their operations. With rising healthcare costs, payers are increasingly pressured to manage expenses while maintaining quality care. This demand for cost efficiency drives the adoption of advanced network management solutions that streamline processes and reduce administrative burdens. According to recent data, healthcare payers that implement effective network management strategies can achieve up to a 20% reduction in operational costs. This trend indicates a growing recognition of the importance of efficient network management in sustaining profitability and enhancing service delivery.
Regulatory Compliance and Standards
Regulatory compliance remains a critical driver within the Healthcare Payer Network Management Market. As healthcare regulations evolve, payers must adapt their network management practices to meet new standards. Compliance with regulations such as HIPAA and the Affordable Care Act necessitates robust network management solutions that ensure data security and patient privacy. The increasing complexity of regulatory requirements compels payers to invest in technologies that facilitate compliance, thereby enhancing their operational capabilities. It is estimated that organizations prioritizing compliance can reduce the risk of penalties and improve their market positioning, making this a vital aspect of network management.
Shift Towards Value-Based Care Models
The transition to value-based care models is significantly influencing the Healthcare Payer Network Management Market. Payers are increasingly focusing on outcomes rather than services rendered, which necessitates a reevaluation of network management strategies. This shift encourages the integration of performance metrics and patient satisfaction indicators into network management processes. As a result, payers are investing in analytics and reporting tools to assess the effectiveness of care delivery. Data suggests that organizations embracing value-based care can improve patient outcomes while reducing costs, thereby reinforcing the importance of effective network management in this evolving landscape.
Increased Focus on Patient-Centric Care
The emphasis on patient-centric care is becoming a pivotal driver in the Healthcare Payer Network Management Market. Payers are recognizing the need to align their network management strategies with the preferences and needs of patients. This focus on patient engagement and satisfaction is prompting payers to develop more flexible and responsive networks that cater to diverse patient populations. By prioritizing patient-centric approaches, payers can enhance care delivery and improve health outcomes. Data indicates that organizations adopting patient-centric models can see a significant increase in patient retention and satisfaction, underscoring the importance of effective network management in achieving these goals.
Technological Advancements in Network Management
Technological advancements are reshaping the Healthcare Payer Network Management Market, driving innovation and efficiency. The integration of artificial intelligence, machine learning, and big data analytics into network management systems enables payers to enhance decision-making processes and optimize resource allocation. These technologies facilitate real-time data analysis, allowing for proactive management of provider networks and improved patient care coordination. As a result, payers that leverage these advancements can achieve a competitive edge in the market. The ongoing evolution of technology suggests that the Healthcare Payer Network Management Market will continue to expand as organizations seek to harness these tools for better outcomes.