Market Trends
Key Emerging Trends in the Ischemic Stroke Surgery Market
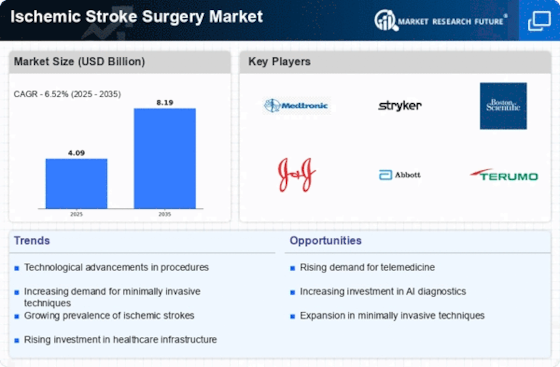
The Ischemic Stroke Surgery market is witnessing dynamic trends that shape the landscape of stroke interventions and contribute to the ongoing evolution of surgical approaches. These trends reflect advancements in technology, changes in patient preferences, and innovations in medical practices. Let's delve into some key trends influencing the Ischemic Stroke Surgery market.
Rise of Endovascular Procedures: Endovascular interventions, such as thrombectomy, have gained prominence in ischemic stroke surgery. The trend towards endovascular procedures is driven by their minimally invasive nature, reduced recovery times, and improved outcomes. This shift represents a departure from traditional surgical methods and a growing reliance on catheter-based techniques to address ischemic strokes.
Integration of Robotics and Navigation Systems: The use of robotics and navigation systems in ischemic stroke surgery is a notable trend contributing to precision and efficiency. Robotic-assisted surgeries allow for enhanced control and accuracy during procedures, reducing the risk of complications. The integration of navigation systems aids surgeons in real-time mapping of the vascular system, guiding their interventions with increased accuracy.
Advancements in Imaging Technologies: Imaging technologies play a pivotal role in ischemic stroke surgery, aiding in diagnosis and guiding surgical interventions. The market is witnessing a trend towards advanced imaging modalities, such as 3D imaging, perfusion imaging, and artificial intelligence (AI)-powered imaging analytics. These technologies provide detailed insights into vascular structures, enabling more informed decision-making during surgery.
Personalized Medicine and Biomarker Research: The trend towards personalized medicine is gaining traction in ischemic stroke surgery. Biomarker research and genetic profiling contribute to tailoring surgical interventions based on individual patient characteristics. This personalized approach aims to optimize treatment strategies, improve patient outcomes, and minimize adverse effects, reflecting a shift towards precision medicine in stroke care.
Telemedicine and Remote Monitoring: Telemedicine has become an integral part of healthcare delivery, including stroke management. The trend towards telemedicine in ischemic stroke surgery involves remote consultations, preoperative assessments, and postoperative follow-ups. Additionally, remote monitoring solutions enable healthcare providers to track patient recovery and intervene promptly if any complications arise.
Focus on Neuroprotective Strategies: Neuroprotective strategies are emerging as a key trend in ischemic stroke surgery. Efforts are directed towards minimizing neuronal damage during and after surgery. Neuroprotective agents and techniques aim to preserve brain function, reduce inflammation, and enhance overall neurological recovery. This trend underscores a holistic approach to ischemic stroke care beyond the surgical intervention itself.
Collaboration and Multidisciplinary Care: Collaborative and multidisciplinary care models are increasingly emphasized in ischemic stroke surgery. The trend involves close collaboration between neurosurgeons, interventional radiologists, neurologists, and rehabilitation specialists. This approach ensures comprehensive care throughout the patient's journey, from diagnosis and surgery to postoperative rehabilitation.
Patient-Centric Care and Shared Decision-Making: Patient-centric care is a growing trend in ischemic stroke surgery, emphasizing shared decision-making between healthcare providers and patients. Informed consent, patient education, and involvement in treatment decisions empower individuals undergoing surgery. This trend aligns with the broader shift towards patient-centered healthcare delivery.
Global Initiatives for Stroke Prevention and Education: Initiatives aimed at stroke prevention and education are influencing trends in ischemic stroke surgery. Global awareness campaigns, community outreach programs, and educational efforts contribute to early detection, timely intervention, and improved outcomes. These initiatives emphasize the importance of preventive measures and prompt medical attention in reducing the burden of ischemic strokes.
Regulatory and Reimbursement Landscape: The evolving regulatory and reimbursement landscape is a trend influencing ischemic stroke surgery. Changes in healthcare policies, insurance coverage, and reimbursement mechanisms impact the accessibility and affordability of surgical interventions. Adapting to these regulatory trends becomes crucial for healthcare providers and manufacturers in the ischemic stroke surgery market.
The Ischemic Stroke Surgery market is characterized by dynamic trends that reflect advancements in technology, a shift towards personalized medicine, and a focus on collaborative and patient-centric care models. These trends collectively contribute to the ongoing refinement of surgical approaches, improving patient outcomes, and shaping the future of ischemic stroke interventions. As the field continues to evolve, staying attuned to these trends will be essential for healthcare professionals, researchers, and stakeholders in the ischemic stroke surgery ecosystem.
















Leave a Comment