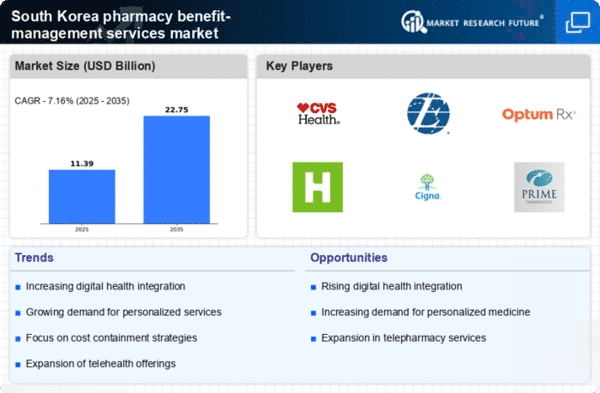
Aging Population
The demographic shift towards an aging population in South Korea significantly influences the pharmacy benefit-management-services market. With projections indicating that by 2025, over 20% of the population will be aged 65 and older, the demand for prescription medications is likely to escalate. Older adults typically require more medications, leading to increased complexity in managing drug benefits. This demographic trend compels healthcare providers and insurers to adopt more sophisticated pharmacy benefit-management strategies to ensure that older patients receive appropriate medications while controlling costs. Consequently, the pharmacy benefit-management-services market is poised for growth as it adapts to the needs of this aging demographic.
Rising Healthcare Expenditure
The increasing healthcare expenditure in South Korea is a pivotal driver for the pharmacy benefit-management-services market. As the government and private sectors allocate more funds towards healthcare, the demand for efficient pharmacy benefit management becomes more pronounced. In 2023, healthcare spending reached approximately 8.1% of GDP, reflecting a growing commitment to health services. This trend suggests that stakeholders are likely to seek cost-effective solutions to manage prescription drug costs, thereby enhancing the role of pharmacy benefit managers. The pharmacy benefit-management-services market is expected to benefit from this rising expenditure, as organizations look to optimize their drug benefit programs and improve patient outcomes.
Increased Focus on Preventive Care
There is a growing emphasis on preventive care within the South Korean healthcare system, which serves as a significant driver for the pharmacy benefit-management-services market. As healthcare providers and insurers recognize the value of preventive measures, there is a shift towards managing chronic conditions before they escalate. This proactive approach often involves the use of medications that can prevent complications, thereby reducing overall healthcare costs. The pharmacy benefit-management-services market is likely to expand as organizations implement programs that promote medication adherence and preventive therapies, ultimately aiming to improve health outcomes and reduce hospitalizations.
Regulatory Support for Drug Pricing
Regulatory support for drug pricing in South Korea is a crucial driver for the pharmacy benefit-management-services market. The government has implemented various policies aimed at controlling drug prices and ensuring access to essential medications. These regulations encourage pharmacy benefit managers to develop strategies that align with government initiatives while optimizing drug costs for insurers and patients. In 2023, the government introduced measures that resulted in a 15% reduction in the prices of certain high-cost medications. Such regulatory frameworks not only promote affordability but also enhance the role of pharmacy benefit managers in negotiating better pricing and managing drug formularies effectively.
Integration of Digital Health Solutions
The integration of digital health solutions into the pharmacy benefit-management-services market is transforming how medications are managed and dispensed. With the rise of telehealth and mobile health applications, patients can now access their prescriptions and manage their medications more effectively. This technological advancement appears to enhance patient engagement and adherence to prescribed therapies. In South Korea, the adoption of digital health tools is on the rise, with a reported increase of 30% in telehealth consultations in 2023. As these digital solutions become more prevalent, the pharmacy benefit-management-services market is likely to evolve, offering innovative ways to streamline medication management and improve patient outcomes.