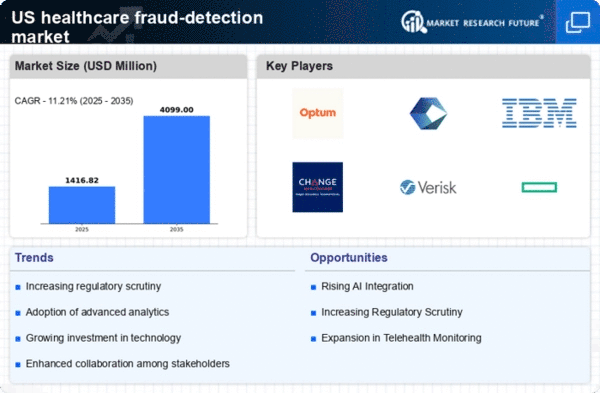
Increased Regulatory Pressure
Increased regulatory pressure is a crucial factor driving the healthcare fraud-detection market. Regulatory bodies, such as the Centers for Medicare & Medicaid Services (CMS), have implemented stringent guidelines to combat fraud and abuse. These regulations necessitate that healthcare providers adopt effective fraud detection measures to ensure compliance. Failure to comply can result in hefty fines and penalties, which further incentivizes organizations to invest in fraud detection solutions. The healthcare fraud-detection market is likely to benefit from this regulatory environment, as organizations seek to align with compliance requirements and avoid potential legal repercussions.
Shift Towards Value-Based Care
The shift towards value-based care is reshaping the landscape of the healthcare fraud-detection market. As healthcare providers transition from fee-for-service models to value-based care, there is an increased emphasis on quality and efficiency. This transition necessitates the implementation of robust fraud detection mechanisms to ensure that providers are reimbursed fairly for the services rendered. the healthcare fraud-detection market is expected to grow as organizations seek to align their practices with value-based care principles. This alignment will enhance their ability to detect and prevent fraudulent activities.
Growing Demand for Cost Reduction
The growing demand for cost reduction in healthcare is a significant driver of the healthcare fraud-detection market. As healthcare costs continue to rise, organizations are under pressure to minimize expenses, including those associated with fraudulent claims. Implementing effective fraud detection systems can lead to substantial savings by preventing losses from fraudulent activities. A study revealed that for every $1 spent on fraud detection, healthcare organizations could save up to $10 in fraudulent claims. This potential for cost savings is likely to encourage more healthcare providers to invest in advanced fraud detection technologies.
Rising Incidence of Healthcare Fraud
The increasing incidence of healthcare fraud in the United States is a primary driver for the healthcare fraud-detection market. Reports indicate that fraudulent activities cost the healthcare system approximately $68 billion annually. This alarming figure has prompted healthcare providers and insurers to invest in advanced fraud detection technologies. The growing awareness of the financial impact of fraud has led to a heightened focus on implementing robust detection systems. As fraudulent schemes become more sophisticated, the demand for innovative solutions in the healthcare fraud-detection market is likely to rise, compelling stakeholders to adopt comprehensive strategies to mitigate risks.
Technological Advancements in Data Analytics
Technological advancements in data analytics are significantly influencing the healthcare fraud-detection market. The integration of big data analytics and machine learning algorithms enables healthcare organizations to analyze vast amounts of data efficiently. This capability allows for the identification of unusual patterns and anomalies that may indicate fraudulent activities. As organizations increasingly rely on data-driven decision-making, the healthcare fraud-detection market is expected to expand. In fact, the market for data analytics in healthcare is projected to reach $50 billion by 2026, underscoring the importance of technology in combating fraud.