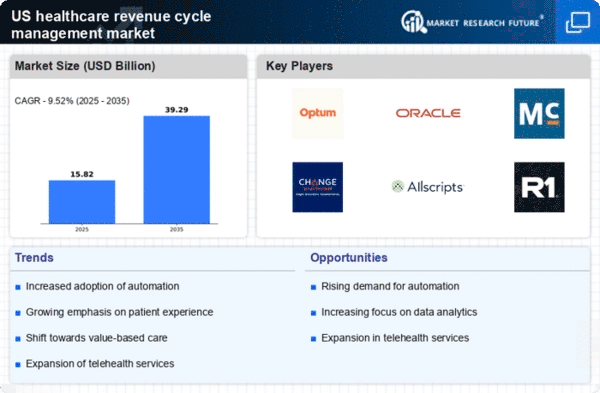
Rising Healthcare Costs
The escalating costs associated with healthcare services in the US are driving the healthcare revenue-cycle-management market. As healthcare expenditures continue to rise, providers are compelled to enhance their revenue cycle processes to ensure financial sustainability. In 2025, healthcare spending in the US is projected to reach approximately $4.5 trillion, which represents a significant increase from previous years. This financial pressure necessitates the adoption of efficient revenue cycle management solutions to optimize billing, collections, and claims processing. Consequently, healthcare organizations are increasingly investing in advanced technologies and services that streamline these processes, thereby contributing to the growth of the healthcare revenue-cycle-management market.
Technological Advancements
Technological advancements are playing a pivotal role in shaping the healthcare revenue-cycle-management market. Innovations such as artificial intelligence (AI), machine learning, and cloud computing are being integrated into revenue cycle processes to enhance efficiency and accuracy. For instance, AI-driven analytics can identify billing errors and optimize claims submissions, potentially reducing denial rates by up to 30%. As healthcare organizations increasingly adopt these technologies, the demand for sophisticated revenue cycle management solutions is expected to grow. By 2025, the integration of technology into revenue cycle processes is likely to become a standard practice, further propelling the healthcare revenue-cycle-management market.
Regulatory Compliance Requirements
The healthcare sector in the US is subject to stringent regulatory compliance requirements, which significantly impact the healthcare revenue-cycle-management market. Regulations such as the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA) mandate that healthcare providers adhere to specific standards for billing and patient data management. Non-compliance can result in substantial financial penalties, prompting organizations to invest in robust revenue cycle management systems that ensure adherence to these regulations. As of 2025, the compliance landscape continues to evolve, necessitating ongoing updates to revenue cycle processes. This dynamic environment creates a sustained demand for healthcare revenue-cycle-management solutions that can adapt to changing regulatory frameworks.
Shift Towards Patient-Centric Care
The ongoing shift towards patient-centric care is influencing the healthcare revenue-cycle-management market. As healthcare providers focus on improving patient experiences and outcomes, they are re-evaluating their revenue cycle processes to align with this new paradigm. This includes enhancing transparency in billing practices and offering flexible payment options to patients. In 2025, it is anticipated that patient engagement strategies will become increasingly integrated into revenue cycle management, leading to improved collections and reduced bad debt. This transformation reflects a broader trend in the healthcare industry, where patient satisfaction is becoming a key performance indicator, thereby driving the demand for innovative revenue cycle management solutions.
Increased Focus on Value-Based Reimbursement
The transition from fee-for-service to value-based reimbursement models is reshaping the healthcare revenue-cycle-management market. As reimbursement structures evolve, healthcare providers are incentivized to deliver high-quality care while managing costs effectively. This shift necessitates a more sophisticated approach to revenue cycle management, as organizations must track and report on various quality metrics. By 2025, it is expected that a significant portion of healthcare reimbursement will be tied to value-based models, compelling providers to invest in revenue cycle solutions that support these new payment structures. This trend not only enhances financial performance but also aligns with broader healthcare goals of improving patient outcomes.























Leave a Comment