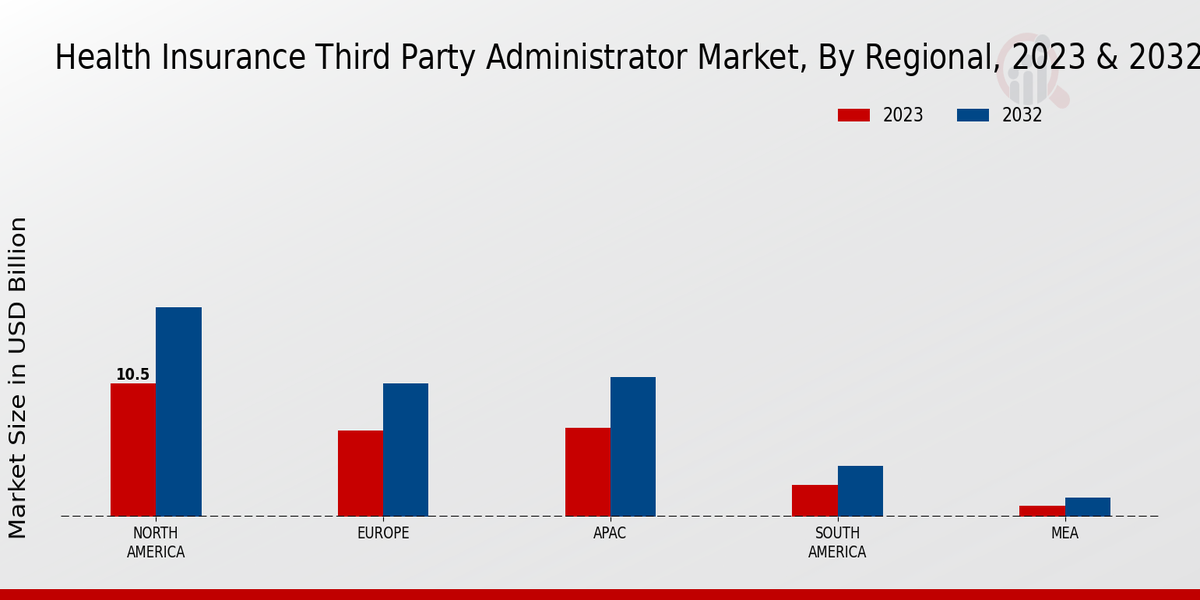
Global Aging Population
The aging population is a critical factor driving the Global Health Insurance Third Party Administrator Market Industry. As life expectancy increases, there is a growing need for comprehensive health insurance solutions tailored to older adults. This demographic shift is prompting insurers to expand their offerings, and third-party administrators are essential in managing these complex insurance products. The increasing prevalence of chronic diseases among the elderly further emphasizes the need for effective health management strategies. As the market is projected to grow from 250 USD Billion in 2024 to 450 USD Billion by 2035, the aging population will likely remain a key driver of demand for third-party administration services.
Market Growth Projections
The Global Health Insurance Third Party Administrator Market Industry is poised for substantial growth, with projections indicating a rise from 250 USD Billion in 2024 to 450 USD Billion by 2035. This growth trajectory suggests a compound annual growth rate of 5.49% from 2025 to 2035. Such figures highlight the increasing reliance on third-party administrators to manage health insurance claims and streamline processes. The expanding market reflects broader trends in healthcare, including rising consumer expectations and the need for efficient service delivery. As the industry evolves, third-party administrators will play an increasingly vital role in shaping the future of health insurance.
Technological Advancements
Technological innovations are reshaping the Global Health Insurance Third Party Administrator Market Industry, enhancing operational efficiency and customer experience. The integration of artificial intelligence, big data analytics, and telemedicine is streamlining claims processing and improving patient engagement. For instance, AI-driven tools can analyze vast amounts of data to identify trends and optimize resource allocation. As these technologies become more prevalent, they are likely to attract investments, contributing to the market's expansion. The anticipated growth from 250 USD Billion in 2024 to 450 USD Billion by 2035 suggests that technology will play a pivotal role in transforming the landscape of health insurance administration.
Rising Healthcare Expenditure
The Global Health Insurance Third Party Administrator Market Industry experiences a notable increase in healthcare expenditure, driven by the growing demand for quality healthcare services. In 2024, the market is projected to reach 250 USD Billion, reflecting a significant investment in health insurance solutions. This trend is likely to continue as governments and private sectors allocate more resources to healthcare, aiming to improve access and quality. As a result, third-party administrators play a crucial role in managing these funds efficiently, ensuring that healthcare providers are compensated promptly and accurately. This dynamic is expected to bolster the market's growth trajectory over the coming years.
Regulatory Changes and Compliance
Regulatory changes are significantly influencing the Global Health Insurance Third Party Administrator Market Industry. Governments worldwide are implementing new policies aimed at enhancing transparency and accountability in health insurance. These regulations often require third-party administrators to adopt more rigorous compliance measures, which can drive operational improvements. For example, the introduction of standardized reporting requirements may lead to increased efficiency in claims processing. As the market adapts to these regulatory frameworks, the demand for third-party administration services is likely to rise, supporting the overall growth of the industry. This evolving landscape underscores the importance of compliance in maintaining competitive advantage.
Increasing Demand for Personalized Healthcare
The shift towards personalized healthcare is a significant driver for the Global Health Insurance Third Party Administrator Market Industry. Consumers are increasingly seeking tailored health plans that cater to their specific needs, prompting insurers to adapt their offerings. This trend is reflected in the rising demand for customized insurance products, which third-party administrators are well-positioned to deliver. By leveraging data analytics, these administrators can create personalized plans that enhance patient satisfaction and improve health outcomes. As the market evolves, the focus on personalized healthcare is expected to contribute to a compound annual growth rate of 5.49% from 2025 to 2035, further solidifying the role of third-party administrators.













Leave a Comment